When to Take Prescription Medications
When to Take Prescription Medications
The best medication to prevent a fracture is related to your personal risk for breaking a bone. That risk is affected by age, prior broken bone(s), family history, smoking and alcohol use, certain medications, your other health conditions, and your risk of falling, just to name a few. It’s also helpful to measure how strong your bones are, typically by means of a bone density test called a DXA (pronounced ‘dex-sah’).
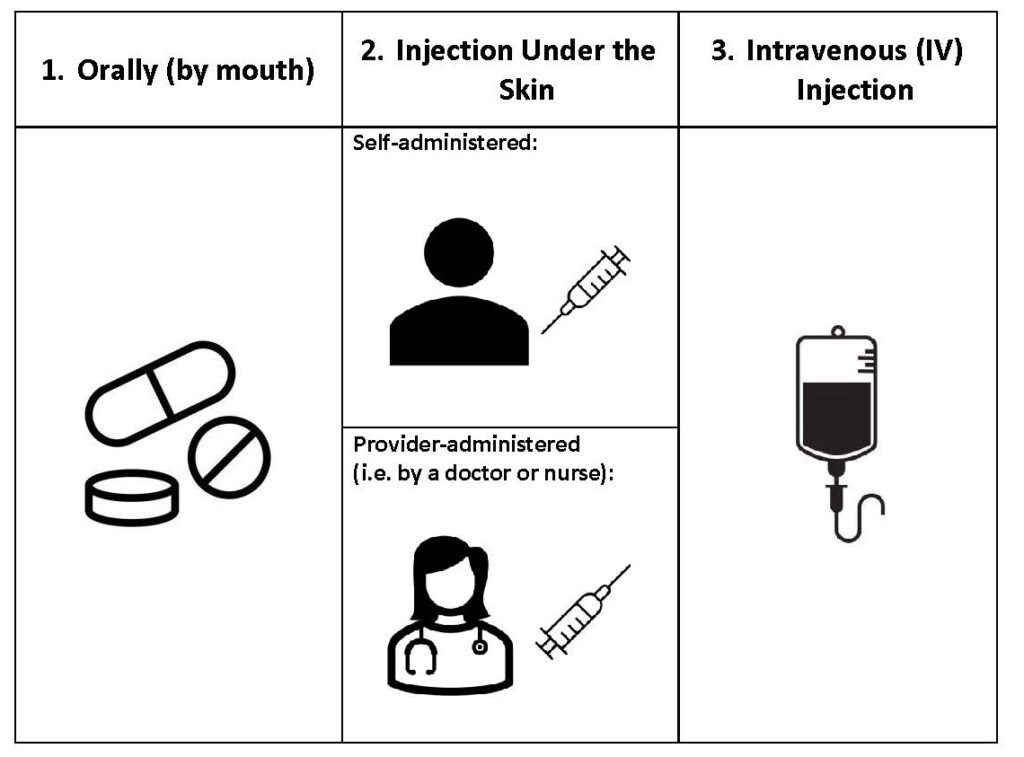
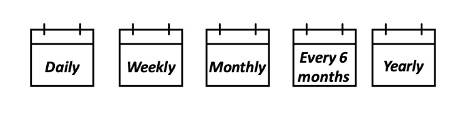
Treatment includes both good nutrition, lifestyle modifications as needed, and for many patients, prescribed medications to help your bones stay strong and healthy. What treatment to use should ultimately be a decision between you and your doctor. The Osteoporosis Medication Treatment Chooser can assist in you and your provider making this decision.
Here are examples of treatment characteristics you should consider in choosing an osteoporosis medication.
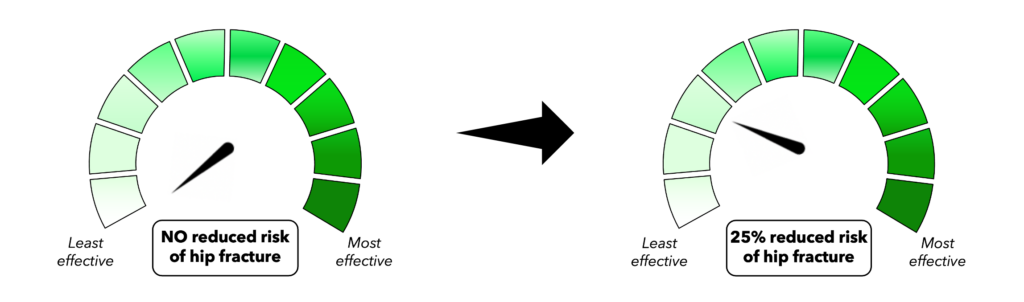
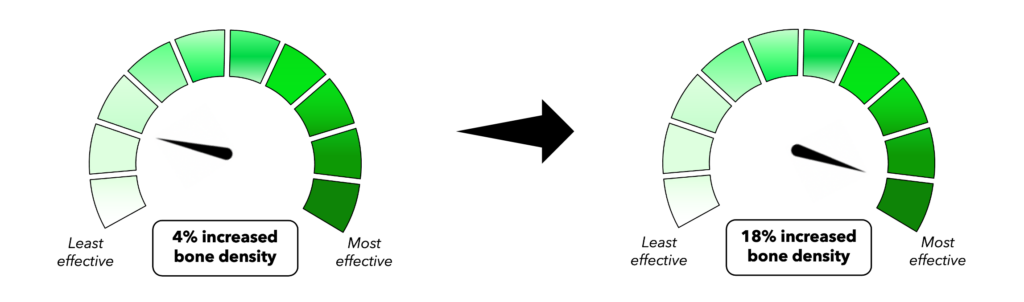
Osteoporosis medical treatments can increase bone density and reduce the risk of developing a new broken bone (fracture). While we want to avoid any new fractures, spine and hip fractures are most common with osteoporosis. A medication’s effectiveness refers to its ability to reduce the risk of fracture and increase bone mineral density.
The gauges below are examples of the range of fracture prevention and the range of improvement in bone mineral density offered by different osteoporosis medicines. Higher percentages mean that the medicine is more effective at preventing fractures and increasing bone density. A 50% reduced risk of spine fracture means that half of all spine fractures (5 out of 10) would be prevented by the medication. A 90% reduced risk of spine fracture means that 9 out of 10 fractures would be prevented by the medication.
Some but not all medications reduce the risk for hip fracture, so the range of effectiveness for hip fracture prevention ranges from 0% to 60%.